
The role of the gut microbiome in osteoporosis and osteoarthritis
A revealing connection
Aleti Institute
9/3/20244 min read


Osteoporosis and osteoarthritis are two of the most common diseases in aging societies. Both diseases are metabolic and significantly affect quality of life, especially in older adults. However, the relationship between these diseases and the gut microbiome has begun to emerge as a crucial topic in current medical research. This article explores how alteration of the gut microbiome may influence the development and progression of osteoporosis and osteoarthritis, and why this relationship could be key to the development of new therapeutic strategies.
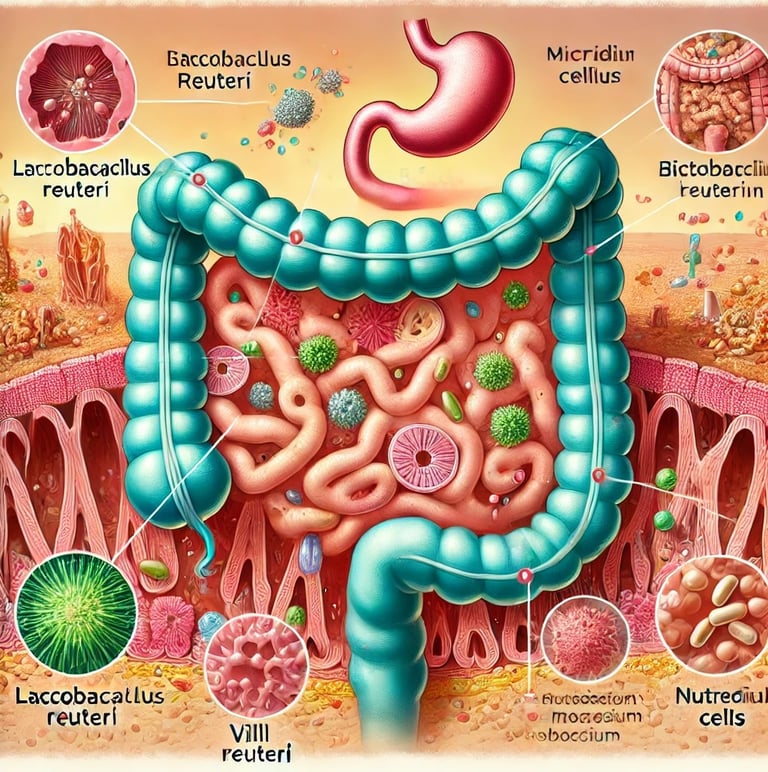
What is the gut microbiome?
The gut microbiome is a diverse community of microorganisms, including bacteria, viruses, and fungi, that inhabit the gastrointestinal tract. These microorganisms play an essential role in various physiological functions, such as nutrient digestion, regulation of the immune system, and protection against external pathogens. Recently, it has been discovered that the gut microbiome is also involved in the regulation of bone metabolism, suggesting that it could have a significant impact on diseases such as osteoporosis and osteoarthritis.
The connection between the gut microbiome and bone health
Numerous studies have shown that the gut microbiome can influence bone health through several mechanisms:
Nutrient absorption: The gut microbiome aids in the absorption of essential minerals and nutrients such as calcium and magnesium, which are crucial for bone formation and maintenance. Bacteria such as Lactobacillus reuteri and Bifidobacterium can promote nutrient absorption by altering gut pH, which in turn can increase bone mineral density.
Intestinal barriers and immune response: The gut microbiome plays a vital role in the formation of the intestinal mucosal barrier, which protects the body against external pathogens. Dysbiosis, or imbalance in the microbiome, can compromise this barrier, increasing serum levels of lipopolysaccharides (LPS) and promoting systemic inflammation. This inflammation can contribute to bone loss and the development of joint diseases.
Hormonal regulation: The gut microbiome also influences the production of hormones that regulate bone metabolism. For example, microbiome-derived peptides, such as glucagon-like peptide 1 (GLP-1) and peptide YY (PYY), play a role in the differentiation of bone mesenchymal cells into osteocytes and adipocytes, directly impacting bone health.
Mechanisms of microbiome depletion in osteoporosis
Osteoporosis is a disease characterized by reduced bone density and an increase in bone fragility, leading to an increased risk of fractures. Depletion of the gut microbiome, whether induced by antibiotic use or germ-free conditions, has been found to affect bone health in several ways:
Intestinal barrier function: Changes in the composition of the gut microbiome can compromise the gut barrier, allowing the passage of macromolecules through the gut wall and altering the absorption of nutrients essential for bone metabolism, such as vitamins B and K, which are crucial for calcium absorption.
Impact on immune function: Depletion of the gut microbiome can affect the immune system, altering the production of pro-inflammatory cytokines such as TNF and interleukin 17, contributing to bone resorption and increasing the risk of osteoporosis
Mechanisms of microbiome depletion in osteoarthritis
Osteoarthritis, a degenerative disease that primarily affects the joints, also appears to be influenced by the gut microbiome. Depletion of the gut microbiome is associated with several changes that can exacerbate osteoarthritis:
Chronic inflammation: Elevated levels of LPS, related to gut dysbiosis, are associated with obesity and metabolic syndrome, which are known risk factors for osteoarthritis. Macrophage activation by LPS can damage joints and increase the severity of knee osteophytes.
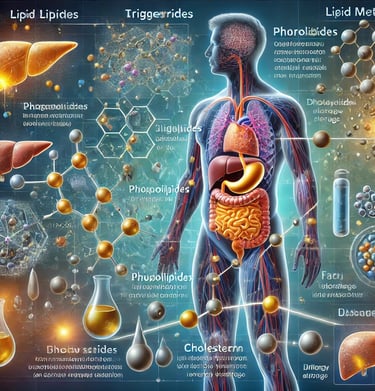
Lipid metabolites: Lipid metabolites play a crucial role in regulating the gut microbiome and may affect systemic inflammation, a key factor in the development of osteoarthritis. Certain microbiome-derived metabolites have been found to alter the production of Wnt signaling-modulating proteins, which may influence the progression of osteoarthritis.
Fecal microbiota transplantation (FMT): This technique, which involves the transfer of gut microbiota from a healthy donor to a recipient, has shown promising results in the management of osteoarthritis. For example, in studies using mouse models, FMT from donors with metabolic syndrome worsened the severity of osteoarthritis, while the opposite results were observed when microbiota from healthy donors was used.
Therapeutic implications and future directions
The growing body of evidence on the role of the gut microbiome in osteoporosis and osteoarthritis suggests that microbiome management could be an effective therapeutic strategy. Probiotic supplementation, for example, has shown potential benefits in improving bone health by regulating luminal pH, increasing mucus production, and modulating the host immune system.
Conclusion:
Research into the relationship between the gut microbiome, osteoporosis, and osteoarthritis is in its early stages, but current findings are promising. Better understanding how gut microbiome disruption affects these diseases could open up new avenues for prevention and treatment. Microbiome genetic testing is a critical tool for personalized patient knowledge. In the meantime, approaches such as probiotic supplementation and fecal microbiota transplantation offer new hope for patients suffering from these debilitating conditions.
In summary, the connection between the gut microbiome and bone health is a rapidly growing area of research, with the potential to transform the way we understand and treat metabolic diseases such as osteoporosis and osteoarthritis.
